Research
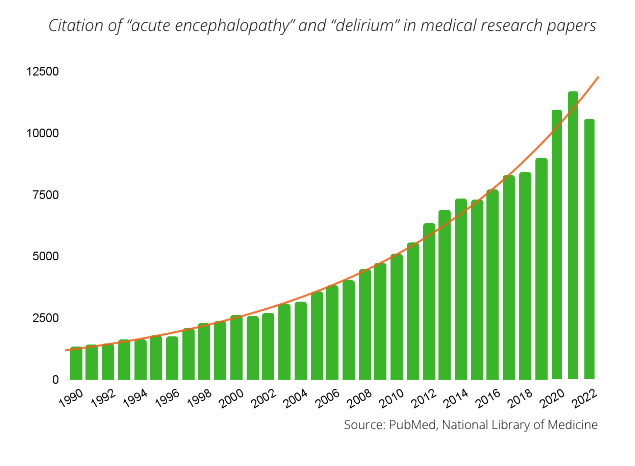
Awareness for Acute Encephalopathy and Delirium Has Seen a Strong Increase
The severity of acute encephalopathy and delirium is increasingly recognized. This is reflected in the enormous increase in the number of publications on this topic. Acute encephalopathy and delirium were only mentioned in roughly 2,500 citations in 2002, but that number rose to over 10,000 by 2022. We developed DeltaScan to meet the clinical need for improved and early detection of delirium. Listed below are several publications that encouraged us to get a better grip on delirium.
Use the filters below to browse publications
The Delphi Delirium Management Algorithms. A practical tool for clinicians, the result of a modified Delphi expert consensus approach.
AwarenessIn 2023, Ottens et al. A panel of 37 internationally recognized delirium experts designed a set of three delirium treatment algorithms. For ward patients, patients after cardiac surgery and for patients in the intensive care unit. The set of algorithms support healthcare providers in the management of underlying EEG changes that are seen in acute encephalopathies underlying delirium.
DeltaScan for the Assessment of Acute Encephalopathy and Delirium in ICU and non-ICU Patients, a Prospective Cross-Sectional Multicenter Validation Study
detectionIn 2023, Ditzel et al. Published the results of a prospective cross-sectional study in 494 patients. The diagnostic accuracy of DeltaScan was investigated. This large and robust study proved that DeltaScan can accurately diagnose acute encephalopathy manifesting as delirium within a few minutes at the patient’s bedside.
Routine use of the confusion assessment method for the intensive care unit
detectionIn 2011, Van Eijck, Slooter et al. examined how delirium screening instruments performed in daily clinical practice. The results demonstrated a low sensitivity of 47%. In the case of hypo-active delirium – the most prevalent form – the sensitivity was only 31%. This formed the motivation to develop an objective screening instrument.
Recognition of Delirium in Postoperative Elderly Patients: A Multicenter Study
detectionIn 2017, Numan et al. published a study demonstrating how difficult it is to recognise delirium. The gold standard for the diagnosis of delirium is an evaluation by a delirium expert. In 21% of the cases these experts differed in their opinions. Only 32% of the actual cases of delirium were recorded in the nursing files, which points to under-detection of delirium in clinical practice. There is a clear need for a user-friendly, reliable method to recognise delirium in clinical practice. EEG could potentially serve as an objective screening method for delirium.
Delirium detection using relative delta power based on 1 minute single-channel EEG: a Multicenter Study
EEGIn 2019, Numan et al. published results which demonstrate that it is possible to diagnose delirium in older post-operative patients using an automatically analysed 1-channel EEG. This method could facilitate objective screening of delirium, in which the result is not dichotomised but instead provides a continuous scale.
Diagnostic Performance and Utility of Quantitative EEG Analyses in Delirium: Confirmatory Results From a Large Retrospective Case-Control Study
EEGIn 2019, a study by Fleischmann et al. demonstrated that a combination of several EEG electrodes can be used for accurate identification and diagnosis of patients with delirium in a mixed cohort of several thousand patients. The diagnostic performance of qualitative EEG exceeded that of classical clinical delirium tests, despite the absence of a priori information about the condition of the patient.
Clinical EEG slowing correlates with delirium severity and predicts poor clinical outcomes
EEGIn 2019, Kimchi et al. demonstrated that EEG retardation detected in clinical practice was correlated to the severity of delirium and was a predictor of unfavourable clinical outcomes, such as prolonged hospitalisation, poorer functional outcomes and increased mortality.
Updated nomenclature of delirium and acute encephalopathy: statement of ten Societies
AwarenessIn 2021, Slooter et al. published a position paper that urges to end segregation between acute encephalopathy and delirium under the title “Updated nomenclature of delirium and acute encephalopathy: statement of ten Societies“.
An automated EEG algorithm to detect polymorphic delta activity in acute encephalopathy presenting as postoperative delirium
EEGIn 2022 Ditzel et al. published that automated polymorphic delta activity detection in 1-channel EEG [ed.: DeltaScan algorithm] had high sensitivity and specificity for acute encephalopathy and delirium.
Delirium in Hospitalized Older Adults
DetectionA large meta-analysis by Marcantonio (USA) in 2017 concluded that up to 75% of the patients had a hypo-active or silent delirium and that only 12% to 35% of delirium patients are diagnosed. The patients that do receive a diagnosis are mainly those with hyperactive delirium
Delirium in critically ill patients: Impact on long-term health-related quality of life and cognitive functioning
AwarenessVan den Boogaard et al. (NL) demonstrated that the cognitive problems following hospitalisation were significantly higher in patients who had suffered delirium, compared to patients without delirium.
Breakthroughs in acute encephalopathy and delirium research
The severity of acute encephalopathy and delirium is increasingly recognized. This is reflected in the enormous increase in the number of publications on these topics. Acute encephalopathy and delirium were only mentioned in roughly 2,500 citations in 2002, but that number rose to over 10,000 by 2022. We developed DeltaScan to meet the clinical need for improved and early detection of delirium. Listed below are several publications that encouraged us to get a better grip on delirium.
In 2010, Heymann (DE) demonstrated that treating delirium too late results in worse outcomes for the patient (
 ). In 2011, Leslie and Inouye (USA) determined that the healthcare costs attributable to delirium are so high that they are ranked between the costs for diabetes and cardiovascular diseases (
). In 2011, Leslie and Inouye (USA) determined that the healthcare costs attributable to delirium are so high that they are ranked between the costs for diabetes and cardiovascular diseases (
 ). In 2013, Pandharipande, Ely et al. (USA) demonstrated that a longer duration of delirium is associated with more significant long-term cognitive deterioration (
). In 2013, Pandharipande, Ely et al. (USA) demonstrated that a longer duration of delirium is associated with more significant long-term cognitive deterioration (
 ). Ely (
). Ely (
 ) and later Pisani (
) and later Pisani (
 ) demonstrated that each day that delirium persists is independently associated with an increase in mortality risk by 10%.
) demonstrated that each day that delirium persists is independently associated with an increase in mortality risk by 10%.
Slooter (NL) has demonstrated that delirium results in worse outcomes in many cases and that this deterioration is independent of the severity of the underlying disease (
 ). As early as 2001, Marcantonio (USA) and others had determined that intensive screening by geriatric specialists can limit the burden of delirium (
). As early as 2001, Marcantonio (USA) and others had determined that intensive screening by geriatric specialists can limit the burden of delirium (
 ). However, Slooter (NL) and others demonstrated in 2011 that the screening instruments currently in use in daily practice in the intensive care units have a poor sensitivity (47%) (
). However, Slooter (NL) and others demonstrated in 2011 that the screening instruments currently in use in daily practice in the intensive care units have a poor sensitivity (47%) (
 ).
).
A large meta-analysis by Marcantonio (USA) in 2017 concluded that up to 75% of the patients had a hypo-active or silent delirium and that only 12% to 35% of delirium patients are diagnosed. The patients that do receive a diagnosis are mainly those with hyperactive delirium (
 ). Inouye et al. (USA) described in 2014 that suffering from delirium not only contributes to a higher risk of mortality, but also to an increased risk of admission to a nursing home due to loss of ADL functionalities (
). Inouye et al. (USA) described in 2014 that suffering from delirium not only contributes to a higher risk of mortality, but also to an increased risk of admission to a nursing home due to loss of ADL functionalities (
 ).
).
In 2010, Martin et al. (USA) studied the relationship between delirium and (post-operative) sepsis, in which they stated that delirium is an independent predictor of sepsis (
 ). Van den Boogaard et al. (NL) demonstrated that the cognitive problems following hospitalisation were significantly higher in patients who had suffered delirium, compared to patients without delirium (
). Van den Boogaard et al. (NL) demonstrated that the cognitive problems following hospitalisation were significantly higher in patients who had suffered delirium, compared to patients without delirium (
 ). Mulkey et al. (USA) recently described the use of EEG in the detection of delirium, stating that EEG – with use of the latest techniques – allows for earlier and improved detection of delirium (
). Mulkey et al. (USA) recently described the use of EEG in the detection of delirium, stating that EEG – with use of the latest techniques – allows for earlier and improved detection of delirium (
 ).
).
Interested? Let's get in touch!
Get in touch to learn how you can reshape acute encephalopathy and delirium care delivery
pageversion: 1.0















